How I Caught My Lipid Problem Early — And What Changed Everything
High lipids don’t scream — they whisper. For years, I felt fine, until a routine check revealed troubling numbers. That moment changed everything. Early intervention isn’t about fear; it’s about awareness. What you do *before* symptoms appear can shape your long-term health. This is how I took control — not with drastic measures, but with simple, proven steps that made a real difference. The truth is, millions live with elevated cholesterol and triglycerides without knowing it. These silent imbalances creep in over time, often unnoticed, until they contribute to serious cardiovascular events. But here’s the good news: when caught early, lipid disorders are highly manageable through lifestyle adjustments supported by medical guidance. This journey isn’t about perfection. It’s about progress, consistency, and making choices today that protect your heart tomorrow.
The Silent Signal: Why Lipid Issues Fly Under the Radar
One of the most dangerous aspects of high lipid levels is their invisibility. Unlike conditions that cause pain, fatigue, or obvious physical changes, elevated cholesterol and triglycerides typically produce no symptoms. People often assume that if they feel well, their body must be functioning optimally. This misconception can delay detection for years, sometimes until a cardiac event occurs. Yet, during that asymptomatic period, damage may already be accumulating in the arteries. Fatty deposits, known as plaques, begin to form along vessel walls, gradually narrowing blood flow and increasing the risk of heart attack or stroke. These changes happen silently, without warning signs, which is why lipid disorders are sometimes called “silent killers.”
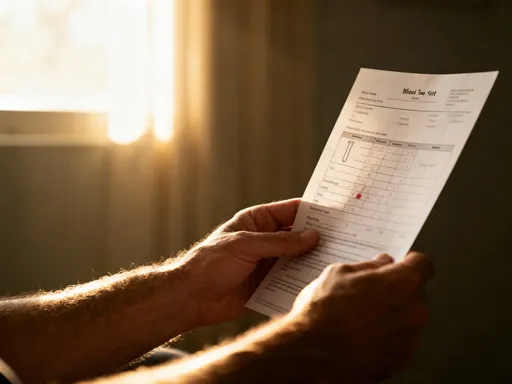
Because the body does not send urgent signals, the only reliable way to detect a lipid problem is through routine blood testing. A standard lipid panel measures total cholesterol, LDL (low-density lipoprotein), HDL (high-density lipoprotein), and triglycerides. For many adults, especially those over 40 or with a family history of heart disease, these tests should be part of regular health screenings every four to six years, or more frequently if risk factors are present. Sedentary lifestyles, diets high in saturated and trans fats, excess weight, and certain medical conditions like diabetes increase the likelihood of developing dyslipidemia, making proactive monitoring even more essential.
Consider the case of a woman in her early 50s who maintained a busy schedule, felt energetic, and believed she was in good health. During a routine physical, her doctor ordered a lipid test as part of a preventive checkup. The results showed elevated LDL and triglycerides, despite her lack of symptoms. Further evaluation revealed early signs of arterial stiffness, a precursor to more serious cardiovascular issues. Because the condition was identified early, she was able to make targeted lifestyle changes and begin appropriate monitoring, avoiding the need for medication at that stage. This scenario underscores a critical point: feeling fine does not guarantee internal health. Relying solely on how you feel can lead to missed opportunities for early intervention.
Another common barrier to detection is the assumption that lipid problems only affect older individuals or those with obvious risk factors like obesity. However, younger adults, even those who appear fit, can have genetic predispositions such as familial hypercholesterolemia, which causes high cholesterol regardless of diet or exercise. Without testing, these individuals may remain unaware until a cardiovascular event occurs. Regular screening removes guesswork and empowers individuals with knowledge. It shifts the focus from reactive care to preventive action, allowing for timely adjustments before irreversible damage takes place. Awareness, not alarm, should be the goal — and regular blood work is the foundation of that awareness.
Why Early Action Beats Late Treatment
The benefits of addressing lipid imbalances early cannot be overstated. Research consistently shows that prolonged exposure to high LDL cholesterol and triglycerides significantly increases the risk of atherosclerosis, the buildup of plaque in the arteries. Over time, this plaque can harden and narrow the arteries, restricting blood flow to the heart and brain. When a clot forms or a piece of plaque breaks off, it can trigger a heart attack or stroke. The longer these lipid abnormalities persist, the greater the cumulative damage. Studies indicate that individuals with untreated high cholesterol for more than a decade face up to three times the risk of coronary artery disease compared to those who manage their levels effectively.
Early intervention disrupts this progression. When lipid imbalances are detected and addressed in their initial stages, the body has a greater capacity to respond. Arterial walls are more resilient, inflammation is lower, and metabolic processes function more efficiently. Small, consistent changes in diet, physical activity, and stress management can lead to measurable improvements in lipid profiles within months. In contrast, waiting until symptoms appear often means the disease has advanced, requiring more aggressive treatments such as high-dose statins, invasive procedures, or long-term medication regimens. At that point, the focus shifts from prevention to damage control.
Moreover, early action preserves quality of life. Managing lipids through lifestyle before complications arise means avoiding the physical limitations, medical appointments, and emotional toll associated with heart disease. It also reduces healthcare costs over time. A study published in the Journal of the American Heart Association found that preventive strategies for cardiovascular risk, including lipid management, could reduce long-term medical expenses by up to 30% compared to treating established disease. This makes early detection not only a health imperative but also a practical one.
The body’s ability to heal and adapt is strongest when imbalances are caught early. For example, reducing LDL cholesterol by just 1 mmol/L (about 39 mg/dL) has been associated with a 20–25% reduction in major vascular events over five years. When implemented early, such reductions are more achievable through moderate lifestyle changes rather than pharmaceutical intervention alone. This window of opportunity — the period before symptoms emerge — is when individuals hold the most power over their health outcomes. Waiting until a crisis occurs means relinquishing that control. Proactive care, grounded in regular monitoring and informed choices, offers a far better path forward.
Food Swaps That Actually Work (No Extreme Diets Needed)
One of the most effective ways to improve lipid levels is through strategic dietary changes. The key is not extreme restriction or trendy diets, but sustainable, science-backed food swaps that support heart health. The foundation of a lipid-friendly diet involves reducing intake of saturated and trans fats while increasing consumption of fiber, healthy fats, and plant-based nutrients. These adjustments don’t require eliminating entire food groups or spending hours in the kitchen. Instead, they focus on smarter choices that fit into everyday life.
Start by replacing processed and fried foods with whole, minimally processed alternatives. For instance, instead of packaged cookies or pastries containing hydrogenated oils, choose fresh fruit with a handful of unsalted nuts. Rather than frying foods in butter or lard, use olive oil or avocado oil for cooking. These oils are rich in monounsaturated fats, which have been shown to lower LDL cholesterol while maintaining or even raising HDL, the “good” cholesterol. Similarly, swapping red meat for fatty fish like salmon, mackerel, or sardines twice a week introduces omega-3 fatty acids, which help reduce triglyceride levels and decrease inflammation in the body.
Another powerful change is increasing dietary fiber, particularly soluble fiber. Found in oats, beans, lentils, apples, and flaxseeds, soluble fiber binds to cholesterol in the digestive system and helps remove it from the body before it enters the bloodstream. Eating just 5 to 10 grams of soluble fiber per day can lower LDL cholesterol by 5 to 10%. A simple breakfast of oatmeal topped with berries and chia seeds provides both fiber and antioxidants, supporting overall cardiovascular health. Replacing white bread and refined grains with whole grain versions adds more fiber and nutrients without sacrificing taste or convenience.
It’s also important to be cautious with so-called “low-fat” or “fat-free” packaged foods. Many of these products compensate for flavor by adding sugar, refined carbohydrates, or artificial ingredients, which can actually worsen triglyceride levels. Instead of relying on processed substitutes, focus on naturally low-fat, nutrient-dense foods like vegetables, legumes, lean poultry, and low-fat dairy. A lunch built around a salad with mixed greens, grilled chicken, avocado, and a vinaigrette made with olive oil offers balanced nutrition that supports healthy lipid metabolism. The goal is not deprivation, but realignment — choosing foods that nourish the body and support long-term heart health.
Movement as Medicine: Finding the Right Rhythm
Physical activity plays a crucial role in regulating lipid levels. Regular exercise influences all components of the lipid profile: it helps lower LDL cholesterol and triglycerides while raising HDL cholesterol. Unlike medications, which target specific markers, movement improves overall metabolic function, enhances circulation, and supports weight management — all of which contribute to better cardiovascular health. The good news is that intense workouts are not required to see benefits. Moderate, consistent activity is often more effective and sustainable in the long run.
Brisk walking for 30 minutes most days of the week is one of the most accessible and well-researched forms of exercise for improving lipid profiles. Studies show that walking at a moderate pace can reduce triglycerides by up to 20% and increase HDL by 4 to 8% over time. For those with limited time, breaking activity into shorter sessions — such as three 10-minute walks — still offers cardiovascular benefits. The key is consistency. Over months, regular movement leads to gradual but meaningful improvements in lipid levels and overall heart function.
In addition to aerobic activity, strength training two to three times per week enhances muscle mass, which in turn improves insulin sensitivity and fat metabolism. Simple bodyweight exercises like squats, lunges, and resistance band routines can be done at home with minimal equipment. These activities not only support lipid regulation but also help maintain bone density and functional strength, especially important as we age. Combining aerobic and resistance training creates a synergistic effect, maximizing cardiovascular and metabolic health.
Common barriers to exercise include lack of time, low energy, or difficulty staying motivated. To overcome these, it helps to integrate movement into daily routines. Taking the stairs, parking farther from store entrances, or doing short stretches during TV commercials all add up. Setting realistic goals, tracking progress, and finding enjoyable activities increase the likelihood of adherence. Walking with a friend, joining a community class, or using a fitness tracker can provide social and psychological support. The goal is not to achieve athletic performance, but to build a rhythm of movement that becomes a natural part of life. Over time, this rhythm transforms from effort into habit, offering lasting protection against lipid-related risks.
Sleep, Stress, and Hidden Triggers
Beyond diet and exercise, two often-overlooked factors significantly influence lipid levels: sleep and stress. Chronic sleep deprivation and persistent psychological stress can disrupt hormonal balance, leading to elevated cortisol levels. Cortisol, the primary stress hormone, affects fat metabolism by promoting fat storage, particularly in the abdominal area, and increasing triglyceride production in the liver. Over time, this contributes to unfavorable lipid profiles and raises cardiovascular risk. Poor sleep quality or insufficient duration — less than seven hours per night — has been linked to higher LDL and lower HDL levels, independent of diet or physical activity.
The connection between stress and lipids operates through multiple pathways. When the body remains in a constant state of alert, it alters how fats are processed and stored. Stress can also lead to unhealthy coping behaviors, such as emotional eating, increased alcohol consumption, or skipping exercise, all of which further impact lipid balance. Similarly, disrupted sleep affects appetite-regulating hormones like leptin and ghrelin, increasing cravings for high-fat, high-sugar foods that worsen cholesterol and triglyceride levels.
Addressing these hidden triggers requires intentional lifestyle strategies. Prioritizing sleep hygiene — maintaining a consistent bedtime, reducing screen exposure before bed, and creating a restful environment — supports deeper, more restorative sleep. Mindfulness practices such as meditation, deep breathing, or gentle yoga can help regulate the nervous system and reduce cortisol levels. Even 10 minutes of daily relaxation exercises have been shown to improve stress resilience and support metabolic health.
Creating boundaries around work, setting aside time for hobbies, and fostering supportive relationships also contribute to emotional well-being. When mental health is prioritized, physical health follows. By recognizing sleep and stress as integral parts of lipid management, individuals gain a more complete picture of heart health. These factors may not appear on a blood test, but they profoundly influence the results. A holistic approach that includes rest and emotional balance is essential for sustainable improvement.
Tracking Progress Without Obsession
Monitoring lipid changes is important, but it must be done with balance. The goal is not to become fixated on numbers, but to use them as tools for informed decision-making. Lab tests, particularly repeat lipid panels, provide objective data on how lifestyle changes are affecting cholesterol and triglyceride levels. Most healthcare providers recommend retesting every three to six months when making significant adjustments, then annually once levels stabilize. These intervals allow enough time to see meaningful trends without encouraging daily anxiety over fluctuations.
It’s important to remember that lipid levels can vary due to factors like recent meals, illness, or stress. A single test should not be interpreted in isolation. Instead, focus on patterns over time. Discussing results with a healthcare provider ensures proper context and prevents self-diagnosis. Doctors can help determine whether changes are due to lifestyle efforts or if additional interventions, such as medication, are needed. Open communication fosters trust and supports shared decision-making.
Avoid relying solely on the scale to measure progress. Weight is just one factor; someone may improve their lipid profile without significant weight loss. Other indicators, such as increased energy, better sleep, or improved clothing fit, also reflect positive changes. The aim is to cultivate a mindset of awareness without anxiety — being informed, not overwhelmed. Regular check-ins with a professional provide reassurance and guidance, helping individuals stay on track without becoming consumed by numbers.
Technology can assist in tracking, but should be used wisely. Apps that log meals, activity, or mood can offer insights, but they should not replace professional advice. The most effective tracking combines objective data with personal experience. When individuals feel better and see lab results improving, motivation naturally increases. This balanced approach supports long-term success without the burnout that comes from obsession.
Building a Sustainable Routine — Not a Quick Fix
Lasting change comes not from short-term fixes, but from sustainable habits. The journey to better lipid health is not about drastic overhauls or temporary diets, but about integrating small, consistent actions into daily life. Environment plays a key role: keeping healthy foods visible and accessible, scheduling regular movement, and creating routines that support good sleep and stress management all increase the likelihood of success. Social support also matters. Sharing goals with family or friends can provide encouragement, accountability, and shared motivation.
Setbacks are normal and should be expected. A holiday meal, a stressful week, or a missed workout does not undo progress. What matters is the ability to return to healthy patterns without guilt or frustration. Flexibility, self-compassion, and persistence are essential qualities. Over time, positive choices become automatic, forming a new normal. The focus shifts from restriction to empowerment — viewing health as a lifelong commitment rather than a destination.
Reflecting on personal experience, the most transformative aspect of this journey was not any single change, but the cumulative effect of many small choices. Choosing water over soda, taking the stairs, preparing a home-cooked meal, or pausing for deep breaths during a busy day — these moments add up. Each one contributes to better lipid regulation and overall well-being. The power lies not in perfection, but in consistency. With awareness, support, and professional guidance, anyone can take meaningful steps toward a healthier future. The best time to start is before symptoms appear — because early action is not just preventive, it is life-changing.
Lipid regulation isn’t just about avoiding disease — it’s about investing in vitality. Catching imbalances early gives you power, not panic. With awareness, small smart choices, and professional guidance, you can build a healthier future. This isn’t a one-time fix; it’s a life-changing shift that starts with a single step — often, before you even feel the need.